Melanoma is the most serious form of skin cancer. It is important to find and treat melanoma before it spreads. With early diagnosis and treatment, melanoma has a high cure rate.
Causes of Melanoma
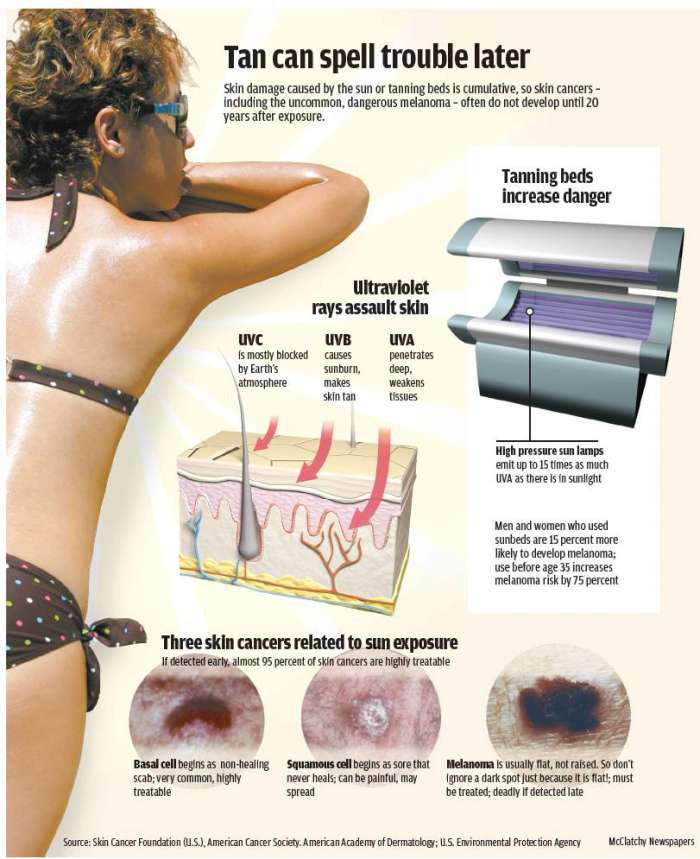
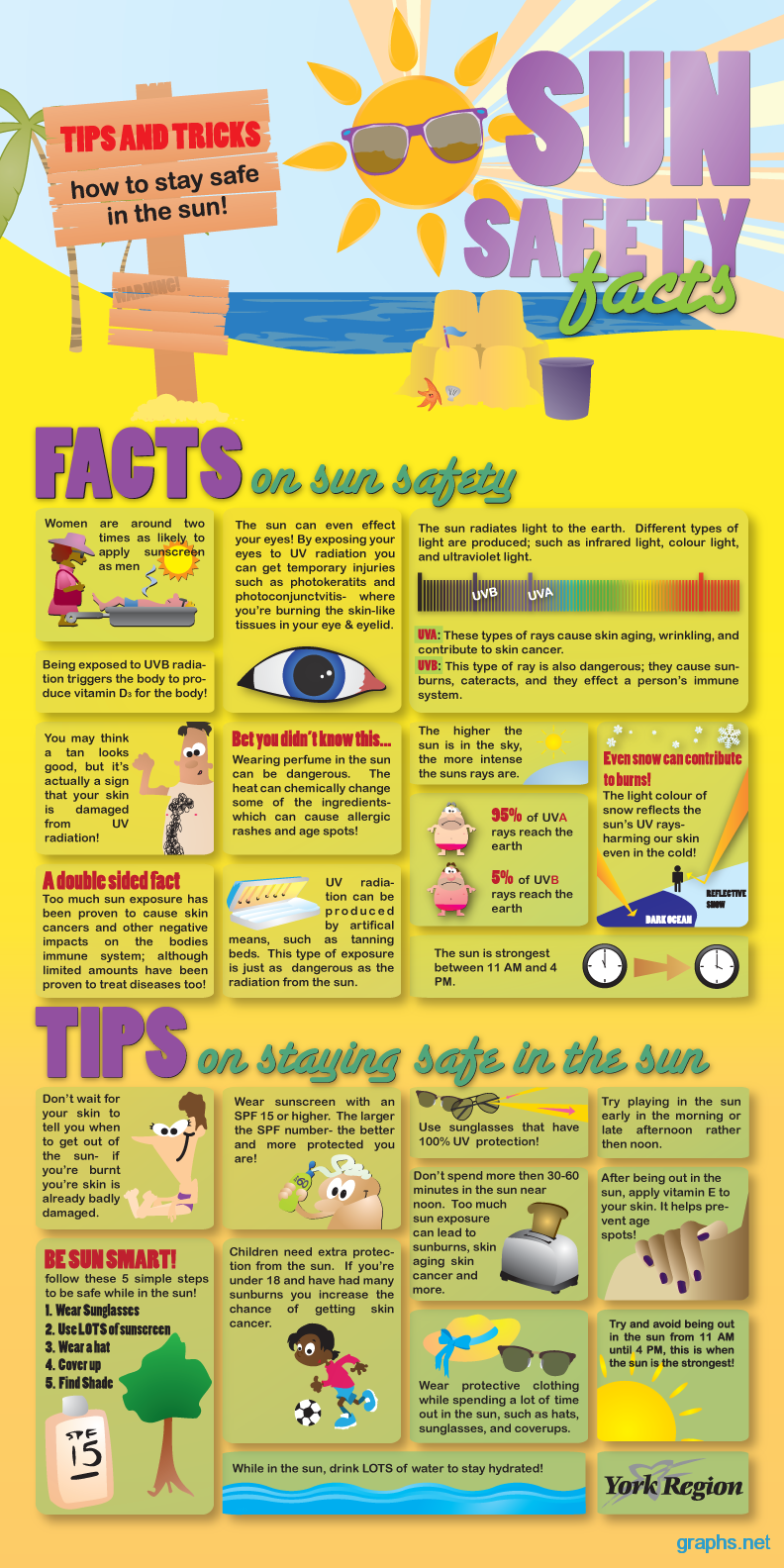
Exposure to UV rays plays a role in developing melanoma, especially in fair skinned people. Many sunburns, especially blistering sunburns, raises the risk of getting melanoma. Not all melanomas are caused by UV radiation. There are other risk factors that increase the likelihood of a person getting melanoma.
Risk Factors for Melanoma
- Fair, sun sensitive skin that tans poorly or burns easily
- Red or blond hair
- Blue or green eyes
- 50 or more small moles
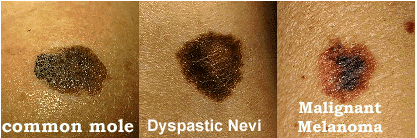
- Unusual looking moles that are often larger than normal and have uneven edges (may be called dysplastic nevi or atypical moles)
- Past sunburns or indoor tanning
- Past history of melanoma or other skin cancer
- Blood relatives who have had melanoma
- Weak immune system, due to disease, organ transplant or medicine
- Age 50 or older
Being younger than 50 does not mean that you cannot get melanoma. It is the most common cancer for young adults age 25-29 years old and the second most common cancer in adolescents and young adults.
Warning Signs of Melanoma

The most common warning sign of melanoma is change. Melanoma may start in an existing mole. A change in shape, color, diameter of a mole can be a sign of melanoma. Other changes to watch out for are moles that begin to itch or bleed.
Not all melanomas start out in a mole. Some melanomas begin suddenly on normal looking skin. A sudden new growth could be melanoma.
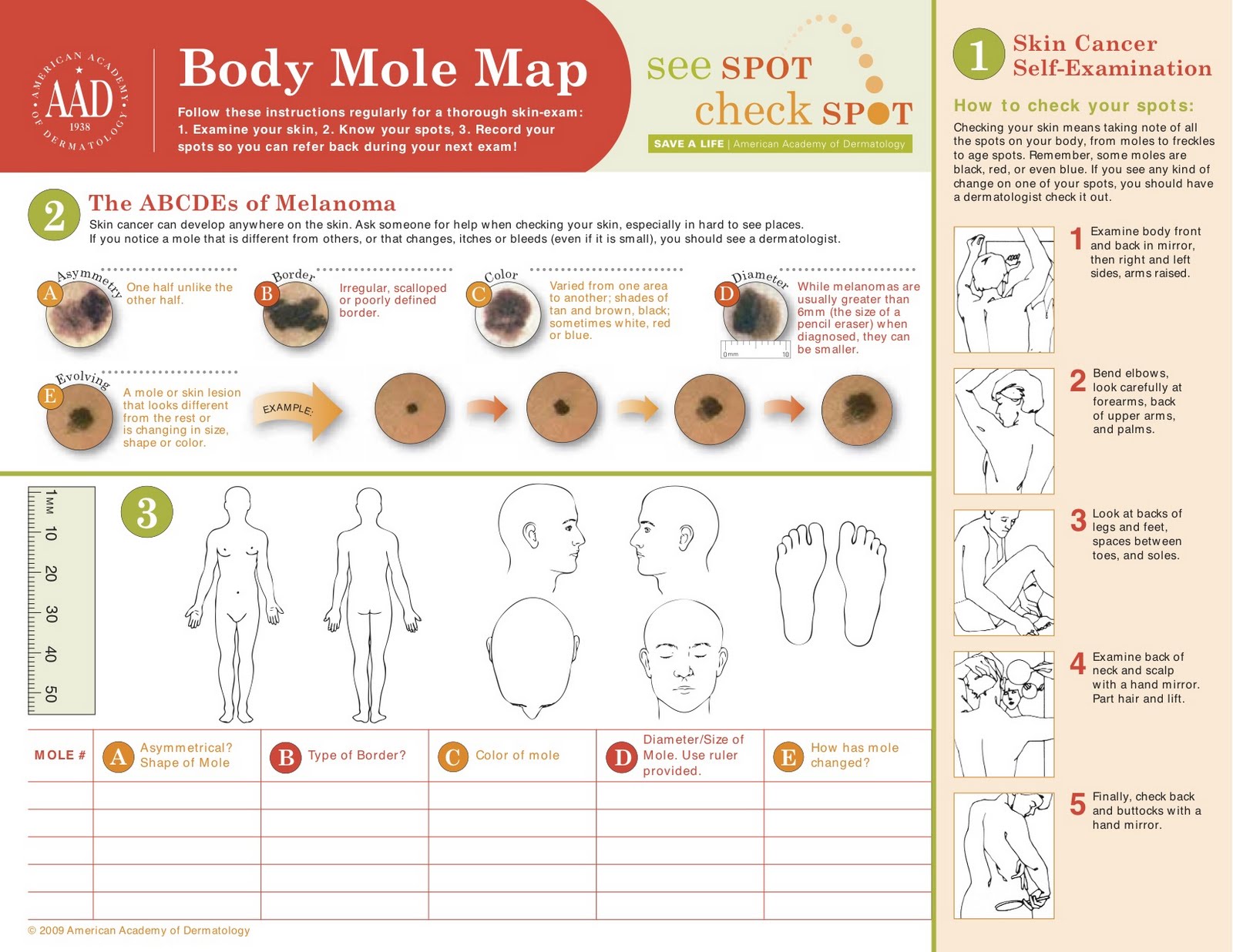
You should perform skin self exams, at least yearly, to look for warning signs. It is helpful to look for the ABCDEs of melanoma detection.
A: Asymmetry – one half does not look like the other half
B: Border – border is irregular, scalloped or poorly defined
C: Color – color is varied from one spot to another; there are shades of tan, brown and black; sometimes, red, white or blue
D: Diameter – melanomas are most often greater than 6 mm or the size of a pencil eraser (but they can be smaller)
E: Evolving – A mole or growth that looks different from the rest or is changing in size, shape or color.

The most likely place for melanoma to appear is on the upper back, torso, lower legs, face, scalp and neck, but can appear anywhere. It can also begin under nails, inside the mouth or on the genitals, and even in your eye.
It is important to remember that melanomas can look different from each other, but the most significant observation is that they look different from your other moles. You can often look for the “ugly duckling” – a mole that looks completely different than the other moles on your body.
If You Find a Mole That Concerns You
Make an appointment for a skin check. If any of the moles are concerning, a biopsy will be performed. During the biopsy, a very small needle is used to inject numbing medication into the skin surrounding the site for the procedure. A sample of skin is then removed and sent to the pathologist for microscopic examination. The pathologist will determine whether or not cancer cells are present and will typically tell what stage the cancer is.
Knowing the stage is important because different stages require different treatments. To determine the stage, it is possible that you could have other testing performed such as ultrasound, x-ray, CT, MRI or PET scans. Sometimes a surgical procedure known as a sentinel lymph node biopsy is necessary to determine the stage. Near by lymph nodes are biopsied to determine whether or not the melanoma has spread. Not all patients will need any or all of these procedures.
Stages of Melanoma
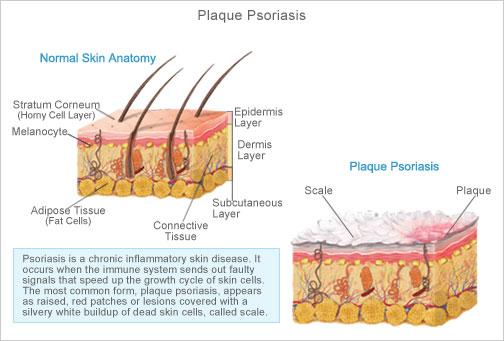
- Stage 0; in situ: Melanoma is confined to the epidermis (top layer of skin)
- Stage I-II: Melanoma is confined to the skin, but has reached the second layer of skin (dermis) or beyond.
- Stage III: Melanoma has spread to nearby lymph nodes.
- Stage IV: Melanoma has spread to the internal organs, beyond the closest lymph nodes or to other lymph nodes or areas of the skin far from the first tumor.
 Treatment of Melanoma
Treatment of Melanoma
Treatment usually starts with excision (surgical removal) of the melanoma and some normal looking skin around it. If taken early enough, this may be the only treatment necessary. The sample is sent to the pathologist, who will determine whether or not cancer cells are in the surrounding skin. If there are no cancer cells present, and the melanoma is in situ, cure rate is near 100%.
If the cancer has spread beyond the skin, more treatment will be needed. This can be more surgery to remove the tumor and radiation or chemotherapy to kill cancer cells. If melanoma is advanced, patients typically receive combination therapy.
Melanoma Can Return
Having melanoma increases your risk for developing new melanomas. They can also recur or return. Melanoma can spread. Because of this, it is essential to keep all appointments and have regular skin checks along with self skin checks at home.
More Information
ABCDEs of Melanoma
Moles
The Sun and Your Skin
Performing Skin Self Checks